Some time back I went on a tangent to rant about the wisdom (or rather, the lack thereof) of concentrating on the public sector for health, to the detriment of the private sector. The word “logistics” was conspicuously absent in that post, a lacuna that I am going to repair in this one.
I guess that it will be clear how important the public sector is for health logistics in developing countries. But how about the private sector? What could be its role?
Combine the words “logistics” and “private sector” in one sentence, and obviously third party logistics (or 3PL) will jump immediately to mind (or it should, if you have all been paying attention and read my post on visibility and transparency). However, there are very few logistics companies (or, for that matter, health ministries or health NGOs) in developing countries who would be able to implement the necessary visibility; so I am afraid 3PL lies rather further in the future than one might wish.
An existing example of more or less successful inclusion of the private sector in the health system, are the private retail pharmacies you can find almost everywhere in developing and middle-income countries. In many of those countries, it would be (almost) impossible to get the necessary medical supplies to the patients without this private initiative.
However, it is not all sunshine and laughter. For example:
- There are serious questions about the quality of the supplied medications by private retail pharmacies in developing countries. Not only can this be extremely harmful for the patients themselves, but it can also contribute to the further spread of resistant strains of viruses, bacteria, and parasites.
- Likewise, the quality of advice given by private pharmacists is not always the best. Research shows that not only is this advice not always up to par due to a lack of knowledge, but there is the obvious problem that the pharmacist wants to sell items on which he can make a (larger) profit; and so they would be clearly tempted to advice e.g. anti-diarrheals instead of ORS.
- Private pharmacies will go where there is profit to make. This means that sparsely populated areas or especially poor populations are more likely not be served by any pharmacy.
- Likewise, private pharmacies will not give away their goods to their poorest customers either. This would mean that the poorest parts of a population that is served exclusively by private pharmacies might not be able to access the necessary medicines.
None of these issues are insurmountable; e.g., quality of supplies and advice can be increased by better supervision and training, incentives can be given to pharmacies to establish themselves in sparsely populated areas, and a voucher system can be instituted to safeguard the needs of the poorest. However, all this costs money too, and in the end it might actually be more effective to have a public (government-owned or sponsored) pharmacy than a public one. This is not something that can be decided on a system-wide level; more likely, the most effective and efficient solution is a mix of private and public pharmacies, supplemented with adequate supervision, training, and financial incentives. Finding the right mix is not an easy task, and probably finding this right mix will include a number of painful mistakes. Don’t forget that the most successful systems in developed countries are the result of many years (and sometimes centuries) of ‘tinkering’.
However, one thing is clear: an all-public system of pharmacies is as likely to be ineffective of hugely inefficient as an all-private system. Dogmatics will not help us at all, and that is as true for pharmacies as for many other issues in health logistics.
(Image courtesy of Getty Images through daylife).












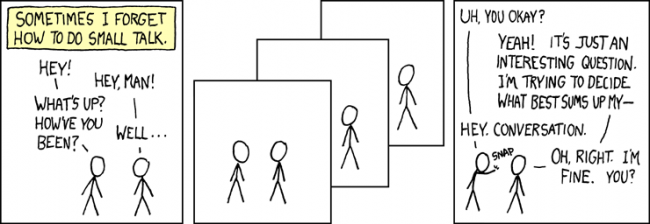
 Sometimes I really wonder why we haven’t seen
Sometimes I really wonder why we haven’t seen 